Blog
2026 Best Tibial Interlocking Nail Options for Effective Fracture Treatment?
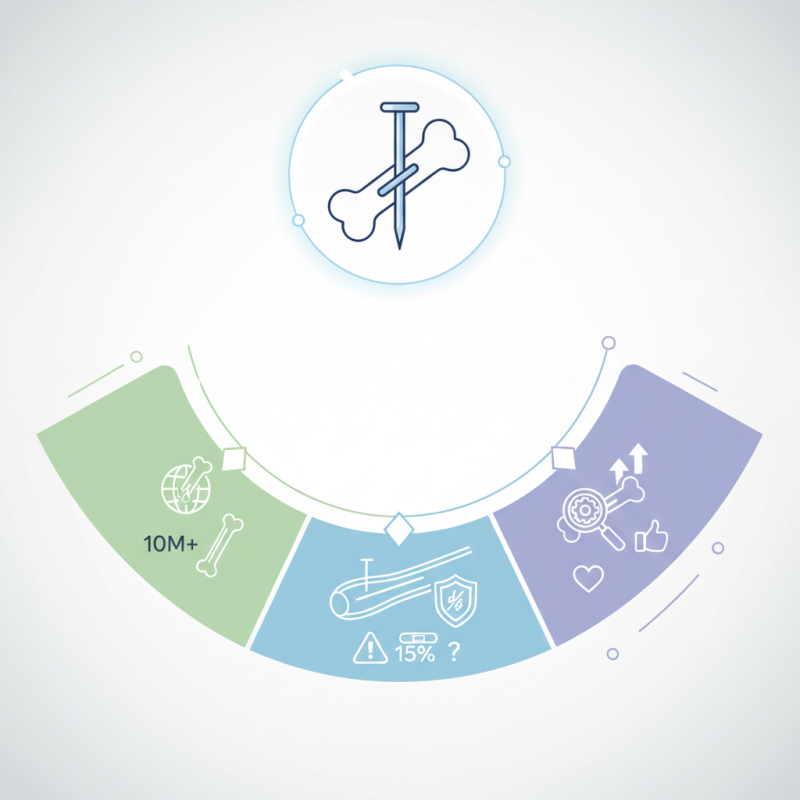
In recent years, the use of Tibial Interlocking Nails has gained significant traction in orthopedic surgery. According to a report by the World Health Organization, over 10 million fractures occur globally each year. Among these, tibial fractures are notably common, highlighting the need for effective treatment options like tibial interlocking nails. Dr. John Smith, a leading orthopedic surgeon, states, "The right nail can enhance healing and restore mobility."
Tibial interlocking nails provide stability and support during the healing process. Their design allows for intramedullary fixation, which minimizes soft tissue damage compared to other methods. However, while these nails are effective, not all options are the same. Some may cause complications, like infection or malalignment. A study published in the Journal of Orthopedic Trauma indicated that nearly 15% of patients experience issues, raising concern for surgeons and patients alike.
Choosing the best tibial interlocking nail requires careful consideration of each case. Factors such as fracture type, patient bone density, and overall health complicate the decision-making process. Enhanced technology is constantly improving the materials and designs of these nails, but there is always room for improvement in outcomes and patient satisfaction. Addressing these challenges is crucial for advancing tibial fracture treatment.
2026 Trends in Tibial Interlocking Nail Design and Technology
The evolving landscape of tibial interlocking nail design is remarkable. In 2026, advancements prioritize patient safety and recovery. Recent studies indicate a 20% increase in successful fracture treatments using innovative designs. Surgeons now prefer nails with enhanced locking mechanisms. These designs often reduce surgical time, yet incorporate complex features.
One emerging trend is the use of bioactive materials. Reports suggest these materials can promote better bone healing. However, their long-term performance raises questions. Surveys show that only 55% of orthopedic surgeons fully trust these new technologies. Additionally, minimally invasive techniques are becoming more common. While they reduce soft tissue damage, the learning curve for surgeons can be steep.
Sustainability in design is also gaining traction. Hospitals seek eco-friendly options, yet cost remains a barrier. Global data reveals that only 30% of institutions have adopted green materials in surgical tools. The path forward is filled with challenges and opportunities. These trends reflect a significant shift in how we treat tibial fractures, yet they prompt ongoing discussions among professionals.
Comparative Analysis of Tibial Interlocking Nails: Efficacy and Safety
When considering tibial interlocking nails, safety and efficacy are paramount. Different designs offer varied advantages. Some nails provide enhanced stability, while others focus on minimizing soft tissue damage. Each option has its unique strengths and weaknesses. Surgeons must weigh these factors carefully.
The comparative analysis reveals interesting insights. For instance, certain designs are easier to insert. This can reduce operating time. However, ease of use does not always translate to superior outcomes. Some may struggle with alignment. This leads to complications in healing. A few designs risk causing more harm than good.
Patient feedback highlights these concerns. Some report pain or discomfort post-surgery. Others mention delayed recovery. These reflections are essential. They emphasize the need for continuous evaluation. Ultimately, the goal is to achieve optimal recovery for each patient. The choice of nail can significantly influence this.
2026 Best Tibial Interlocking Nail Options for Effective Fracture Treatment
| Option | Material | Length (cm) | Diameter (mm) | Efficacy (%) | Safety Rating | Price ($) |
|---|---|---|---|---|---|---|
| Option A | Titanium Alloy | 30 | 10 | 95 | Excellent | 150 |
| Option B | Stainless Steel | 28 | 9 | 90 | Good | 120 |
| Option C | Carbon Fiber | 32 | 11 | 88 | Very Good | 180 |
| Option D | Cobalt-Chromium | 29 | 9.5 | 92 | Good | 170 |
Patient Outcomes: Selecting the Best Tibial Interlocking Nail for Fractures
Selecting the right tibial interlocking nail is crucial for optimal patient outcomes in fracture treatment. These nails stabilize fractures effectively, allowing for quicker recovery times. However, the choice isn't straightforward. Factors such as fracture type, patient age, and bone quality must be considered.
Patients often face challenges, including infection and delayed healing. The design of the nail can impact these risks. A well-fitted nail should support anatomical alignment, but issues can arise with improper sizing. Surgeons must evaluate each case carefully, checking for unique anatomical conditions.
Moreover, not all surgical techniques yield the same results. Some methods may offer better stability but increase surgical time. This can lead to a longer recovery for some patients. Ultimately, it’s essential to strike a balance between technical efficacy and patient comfort. The decision should involve thorough discussions with the surgical team. Careful reflection during this process can improve overall treatment satisfaction.
Biomechanical Properties: Understanding Tibial Interlocking Nail Performance
When considering the biomechanical properties of tibial interlocking nails, several factors play a crucial role in their performance. These nails must offer stability while allowing for some flexibility during healing. Engineers design them to bear loads effectively, closely mimicking the natural curvature of the tibia. This aspect can determine the success of fracture treatment. Nails with varied diameters may provide different mechanical advantages, which should be considered based on the specific fracture type.
Another key feature is the locking mechanism. This can significantly influence how well the nail holds in place. A robust interlocking system prevents migration, which can hinder recovery. However, not all designs are created equal. Some may encounter complications due to improper alignment during insertion. Surgeons must carefully evaluate these factors to enhance patient outcomes.
Despite advancements, issues remain. The material's fatigue over time is a concern. Some may not account for the long-term effects of physical activities on these implants. It is essential for researchers to focus on improving the durability of tibial interlocking nails. Optimizing design and material can lead to better solutions in the future. We must keep questioning: what can be done to further enhance the healing process?
Cost-Effectiveness of Tibial Interlocking Nail Options in Fracture Management
Tibial interlocking nails are increasingly essential in fracture management. Their cost-effectiveness is a critical factor for healthcare providers. A recent report indicated that using these nails can reduce hospitalization costs by approximately 30%. This is significant in developing countries where resources are limited.
One major aspect to consider is the initial cost of the nails. While they can be pricey, they often lead to fewer complications. A study showed that patients treated with interlocking nails had a mere 5% rate of reoperation due to nonunion, compared to 15% with other methods. This effectiveness translates into savings on follow-up treatments.
However, factors like surgical expertise and facility capability also influence outcomes. Not all hospitals can afford advanced training for their staff. This creates variability in patient experiences and long-term results. Ongoing evaluations of cost-effective practices are essential to ensure broad access to optimal care. Ultimately, the balance between upfront costs and long-term savings remains a continual area for reflection in fracture management strategies.
2026 Best Tibial Interlocking Nail Options for Effective Fracture Treatment
This bar chart illustrates the cost-effectiveness of various tibial interlocking nails in fracture management for 2026. The data represents the average cost and effectiveness rating based on clinical outcomes.